Researching a rarity
HOW CAN WE TELL THAT SOMEONE HAS SICKLE CELL ANEMIA?
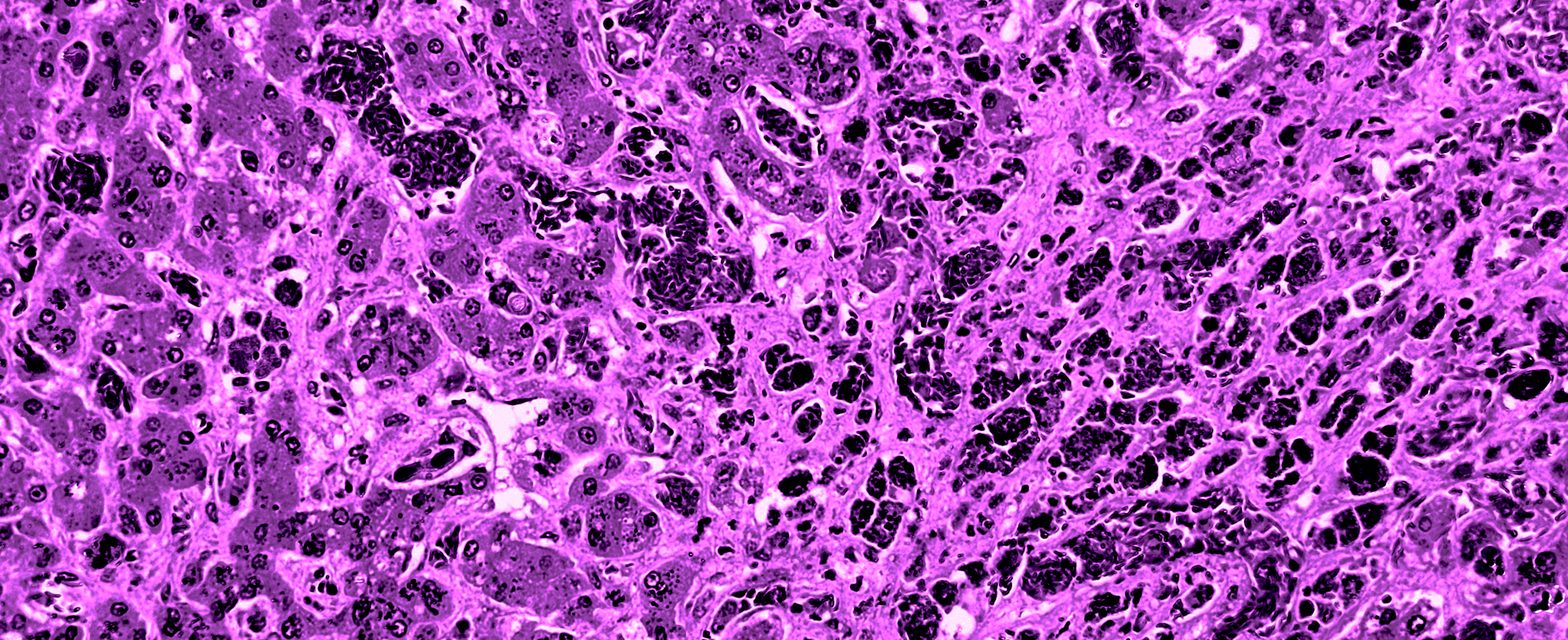
That’s a mystery without an easy answer. The dysfunction and malformation happen deep below the body’s surface. Those who have the disease, a genetically passed-on condition that causes red blood cells to become misshapen, clogging blood vessels and depriving organs of oxygen, bear no outward markers. And the disease itself can’t be detected by the standard diagnostic tools.
The pain mimics other chronic conditions. It is searing; it comes in waves and it is often centered in joints and bones. Known as a sickle cell crisis, the pain can be so severe that a person having an episode often must be hospitalized.
In the United States, the overwhelming number of the estimated 100,000 residents with the disease are African American. One in every 13 Black children is born with the genetic trait, a mutation traced thousands of years back to sub-Saharan Africans’ adaptation to malaria outbreaks.
And there are many false assumptions about the disease. Because of the severity of the pain, opiate analgesics often must be prescribed for relief.
Health care professionals unaware of the disease often mislabel sickle cell patients as addicts in search of drugs for themselves or to sell on the streets.
Another is that, despite statistics showing that people with sickle cell come from every socio-economic level, people who have it are often presumed to be at the bottom.
Because sickle cell is on the list of medical conditions known as “orphan diseases,” meaning those that have not been adopted by institutional researchers or the pharmaceutical industry due to the small numbers of people who would benefit, the disease has remained a scourge since it was discovered in 1910.
Ignoring those numbers and stepping into that breach is The Pittsburgh Foundation, which has awarded a $500,000 grant to boost potentially ground-breaking investigations at the Vascular Medicine Institute of the University of Pittsburgh’s School of Medicine, one of the centers working against the backdrop of the National Institutes of Health to develop a pathway to a cure.
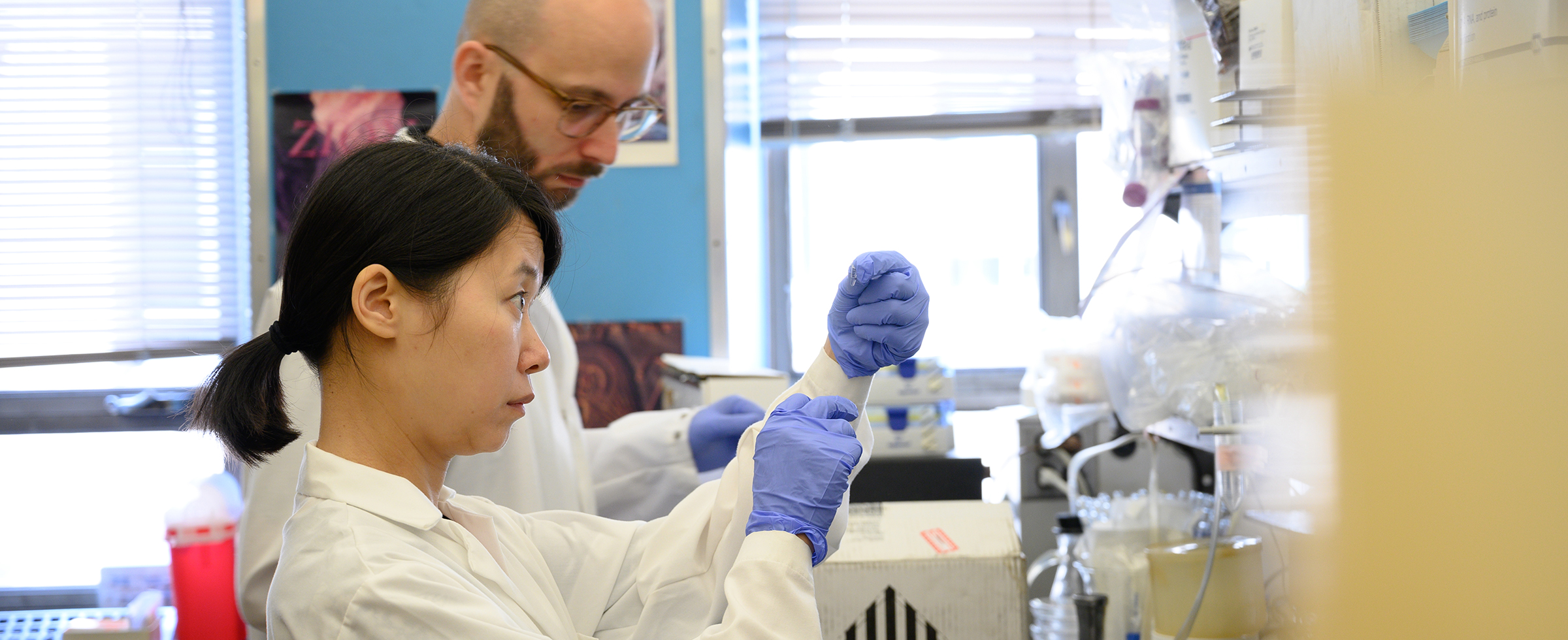
Created a decade ago, the Institute is now directed by Dr. Mark Gladwin, who also leads the university’s Division of Pulmonary, Allergy and Critical Care Medicine and serves as the chair of the Department of Medicine. He has recruited a team of experts from various medical disciplines to spearhead hemolytic research into sickle cell. The immediate goal, he says, is to develop a noninvasive technique for detecting the source of disease flare-ups at the molecular level.
“One fundamental problem related to [sickle cell] pain crisis is that it is not visible,” says Dr. Enrico Novelli, a medical oncologist and hematologist who leads the sickle cell team at VMI. “People may be in pain, but there’s no outward, physical sign that can be seen by medical providers.”

One fundamental problem related to sickle cell pain crisis is that it is not visible. People may be in pain, but there's no outward, physical sign that can be seen by medical providers.
--DR. ENRICO NOVELLI
Key drivers of the team’s research are the recent breakthroughs in nuclear medical tracers and advanced studies utilizing laboratory mice. Dr. Carolyn Anderson, a professor in the Department of Radiology whose expertise includes translating mouse studies into medical protocols appropriate for people, believes that the researchers are very close to being able to accurately and rapidly image the actions that cause sickle cell pain at the molecular level.
“The important thing about this grant is that it is bringing together people like myself and Enrico, who is a clinical medical doctor,” Anderson says. “In nuclear medicine, we image the biochemistry and physiology, so it's a very active process. Changes that happen at a molecular level happen long before you can see changes on an anatomical level.”
Novelli says that a complex network of players is essential to continued progress. “We now have therapies — drugs that target these molecules and these events.”
Because of the research with mouse studies, he says, “there has finally been a revolution in sickle cell disease research. We are on the cusp of a cure by way of treatment that would become widely available.”
The researchers say that The Pittsburgh Foundation grant will move the work more quickly from mouse models to humans. Upcoming multi-center clinical trials will enlist African American adults in western Pennsylvania, Ohio and West Virginia to test the accuracy of the methodology developed at the institute. While about 500 people are currently referred to UPMC for treatment, not all of them will be part of the study.
“If this project is successful,” Novelli says, “it will lead to a better understanding of the disease in humans and restore credibility to the patients who present with pain, and it will improve the relationship between health care providers and patients. It has far-reaching consequences.”
Original story appeared in the Forum Quarterly Spring 2019.